|
Dietrich, a 45 year old man, presents to you at the insistance of his wife, who gives
the history.
She complains that for several years he has been getting "the run-around" from physicians who
cannot seem to nail down his diagnosis. Initially his symptoms were mild and attributed to
"middle age". However, slowly and steadily they have progressed and are now greatly
affecting his life.
Deitrich barely moves during the presentation of the chief complaint, and slumps with his
head down. His wife says that about three years ago, he began noticing slight memory problems and lack of
attention. He breaks in, "Yes, but that's because I don't listen to you because
all you do is nag, nag, nag." The wife resumes, explaining that within the last year both of them noticed balance and
equilibrium issues that caused him to feel dizzy. He went to his primary care physician,
who sent him to an otolaryngologist. After a quick exam, the otolaryngologist diagnosed
benign positional vertigo and performed some inpatient procedures that provided no
relief. The primary care physician then sent him to a psychologist, who diagnosed
post-traumatic stress disorder and said the stumbling was symbolic of forgotten life
trauma. Three months of "visualization therapy" did not help, and Dietrich refused
to continue it.
The primary care physician then prescribed big doses of vitamins. Although his issues with equilibrium were annoying, the patient did not get seriously
worried about the state of his health until six months ago, when he began having significant trouble
walking, standing, and moving in a coordinated manner.
The patient looks frustrated, inattentive, and does not volunteer anything.
The wife carries on about how there must be a cure if you will just look.
Please remember you are a KCUMB alumnus and will practice better medicine.
|
|
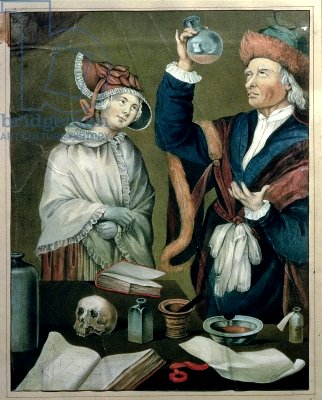
Sansanietto
The High German Doctor
|